CMS announced several changes in Transmittal 10269 regarding billing home infusions effective January 1, 2021. The Medicare Claims Processing Manual, Ch. 32 § 411 et al. has been updated reflecting upcoming changes of home infusion therapy services.
Policy Guidance
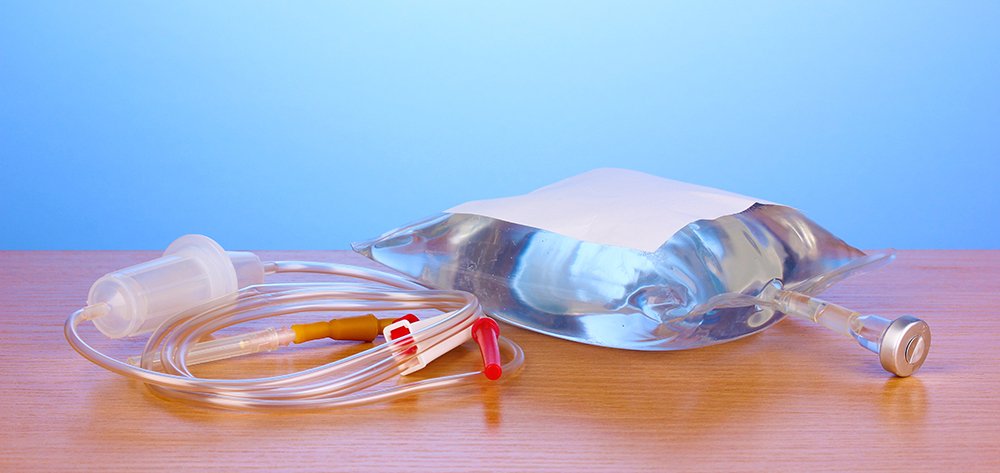
Effective January 1, 2021 home infusion therapy benefit covers professional services inclusive of nursing service in accordance with the plan of care, patient training and education (which are not covered under a DME benefit), remote monitoring, and monitoring for services for the provision of home infusion therapy and home infusion drugs furnished by a qualified home infusion therapy supplier.
The home infusion therapy are services furnished for drug administration on a calendar day. The billing must be reported with the date of service on which the infusion therapy services are furnished. The infusion of the drug therapy must be inherently complex to require the skill performed by, or under the supervision or professional or technical personnel.
Coverage Requirements
Payment for home infusion drug therapy is only reimbursed when certain requirements are met:
- Certain drugs and biologicals administered through an item covered by DME
- Supplier must be enrolled in Medicare as a “qualified home infusion therapy supplier”
- Beneficiary must be under the care of a physician, NP, or PA
- Beneficiary must be under the care of a physician-established plan of care which prescribes the infusion:
- Type
- Amount; and
- Duration of infusion therapy services.
What is not covered
Insulin pump systems or self-administered drugs or biologicals on a self-administered drug are not include under the benefit.
What is covered
Drugs administered through the use of external infusion pumps. The drug is a parenteral drug or biological administered intravenously, or subcutaneously for 15 minutes or more, at home, through a pump that is a DME item.
Billing Requirements
The changes are to capture the professional component along with the drug. “G” codes are billed on claims to the A/B Macs and are payable to home infusion therapy suppliers. Note: This service is no longer payable to DME suppliers. Failure to follow this rule change will results in a denied claim and delayed revenue.
The “J” codes are billed to the DME MACs by the DME supplier. The Type of Service (TOS) Code 1 is reported for the G-codes. Contractors will only pay one of the G-codes per line item date of service when one of the drugs from the applicable category is billed with the same date of service within 30 days prior to the G-code visit.
G-codes on the MPFSE fee file will be “a per day rate.” The units on the line should not be multiplied by the rate. The drug will be separately payable from the G-code line item.
When multiple drug administrations on a calendar day, a single payment will be made that is equal to the highest payment category. This means suppliers can only bill for one visit and should report the highest paying visit with the applicable drug.
Home therapy services may only be reported with one “initial visit” G-code for a new patient who had previously received their last home infusion therapy more than 60 days prior to the new initial home infusion therapy service.
Home infusion therapy visits are reported in 15-minute increments. This means the claim form would have 1 unit for every 15 minutes. If you report units of 15 for a 15-minute service you would be overbilling. Below is a time table when reporting time increments:
| Unit |
Time in minutes |
| 1 | <23 minutes |
| 2 | 23 – 37 |
| 3 | 38 – 52 |
| 4 | 53-67 |
| 5 | 68-82 |
| 6 | 83-97 |
| 7 | 98-112 |
| 8 | 113-127 |
| 9 | 128-142 |
| 10 | 143-158 |
Professional Services G-Codes
The professional services are captured by reporting the appropriate G-code. There are three payment categories of G-codes.
- Payment Category 1: includes certain intravenous antifungals and antivirals, uninterrupted long-term infusions, payment management, inotropic, chelation drugs.
G-Codes used for this category:
Initial Visit: G0088
Subsequent Visit: G0068
- Payment Category 2: includes subcutaneous immunotherapy and other certain subcutaneous infusion drugs.
G-codes used for this category:
Initial Visit: G0089
Subsequent Visit: G0069
- Payment Category 3: includes certain chemotherapy drugs.
G-codes used for this category:
Initial Visit: G0090
Subsequent Visit: G0070
G-code long and short descriptions:
- G0068: Professional services for the administration of anti-infective, pain management, chelation, pulmonary hypertension, inotropic, or other intravenous infusion drug or biological (excluding chemotherapy or other highly complex drug or biological) for each infusion drug administration calendar day in the individual’s home, each 15 minutes
Short Descriptor: Adm IV infusion drug in home
- G0069: Professional services for the administration of subcutaneous immunotherapy or other subcutaneous infusion drug or biological for each infusion drug administration calendar day in the individual’s home, each 15 minutes
Short Descriptor: Adm SQ infusion drug in home
- G0070: Professional services for the administration of intravenous chemotherapy or other intravenous highly complex drug or biological infusion for each infusion drug administration calendar day in the individual’s home, each 15 minutes.
Short Descriptor: Adm of IV chemo drug in home
- G0088: Professional services, initial visit, for the administration of anti-infective, pain management, chelation, pulmonary hypertension, inotropic, or other intravenous infusion drug or biological (excluding chemotherapy or other highly complex drug or biological) for each infusion drug administration calendar day in the individual’s home, each 15 minutes.
Short Descriptor: Adm IV drug 1st home visit
- G0089: Professional services, initial visit, for the administration of subcutaneous immunotherapy or other subcutaneous infusion drug or biological for each infusion drug administration calendar day in the individual’s home, each 15 minutes.
Short Descriptor: Adm SubQ drug 1st home visit
- G0090: Professional services, initial visit, for the administration of intravenous chemotherapy or other highly complex infusion drug or biological for each infusion drug administration calendar day in the individual’s home, each 15 minutes.
Short Descriptor: Adm IV chemo 1st home visit
Documentation & Audit Issues
- The plan of care must:
- Be an established plan of care
- Clearly describe the type of drug
- The amount to be administered
- The duration of the drug therapy
- Bill on Calendar day of drug therapy
- On administration day start and stop times should clearly be documented to capture time correctly.
- Unit billing (professional): Properly report G-code units per 15 minutes and round appropriately.
- Unit billing (drug): Properly report the J-code units based on the HCPCS code description. Not following this can result in over or under reporting
- Signature of the nurse, PA, NP who is administering the drug
- Report initial visits and subsequent visits appropriately
- Report the G-codes to the correct A/B Carrier